Vyaire Medical – Respiratory Care in the COVID-19 Crisis

Last year I interviewed Dr. Christopher Varga about his innovative use of simulation for designing better respiratory care devices at Vyaire Medical. It was a great interview, about an application that is obviously very important; one with direct positive outcomes for often critically ill patients.
However, it wasn’t until the whole world got overtaken by this horrible virus, that I realized just how important. When I reread the opening paragraph of that article (which I was actually quite pleased with at the time), it suddenly looks dated:
Most of us take breathing for granted, taking around 17 to 23,000 breaths per day, mostly without any conscious effort. However, for many reasons, breathing can present a significant challenge to the elderly and infirm. For premature babies, with tiny under-developed lungs, minimizing the effort of breathing is critical, as every calorie of wasted energy expenditure negatively impacts clinical outcomes.
Engineering Innovation #4: “Vyaire Medical: Breathing new life into respiratory care”
It’s fair to say that in April 2020 no one takes breathing for granted. And, in the middle of a COVID-19 pandemic, it’s not just premature babies for whom every calorie wasted struggling for breath can negatively impact clinical outcomes.
Vyaire Medical describes themself as “the leading manufacturer of solutions for the treatment and monitoring of respiratory conditions at every stage of life.” Not only are Vyaire one of the world’s largest producers of respiratory care equipment, but they can also lay claim to being direct descendants of the company that invented and refined the first mechanical ventilator.
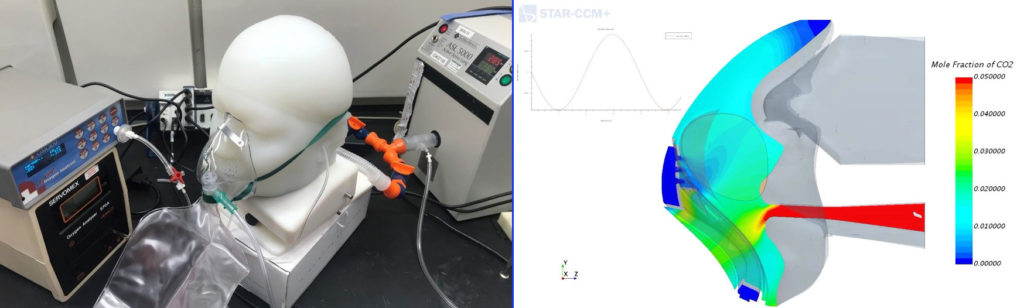
Vyaire’s commitment to supporting patients at “every stage of life” represents a considerable engineering challenge. Not only do patients come in a variety of shapes and sizes (morphologies), but they also breathe in a variety of ways: some people are “mouth breathers,” some are “nose breathers,” most of us breathe using a combination of both. Each patient also has a unique breathing profile, that depends on their lung function and structure.
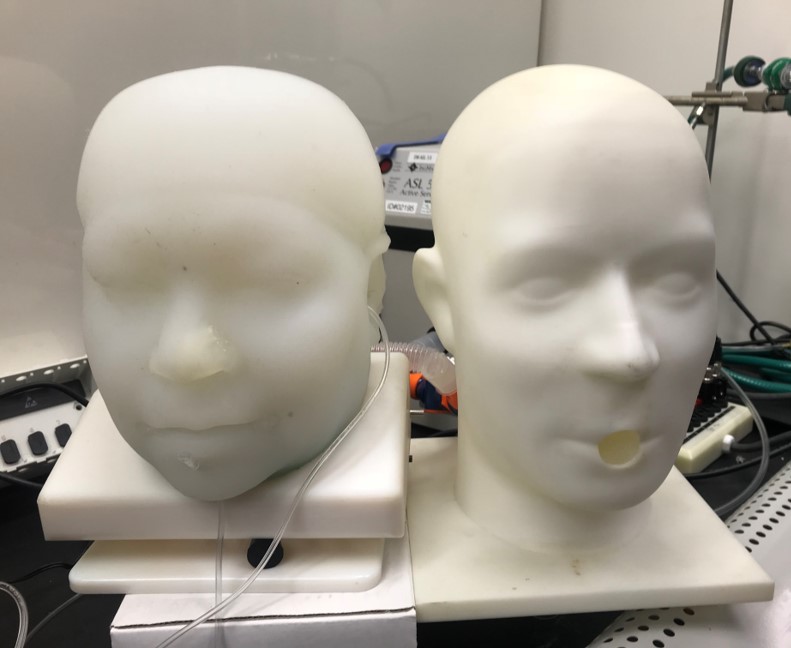
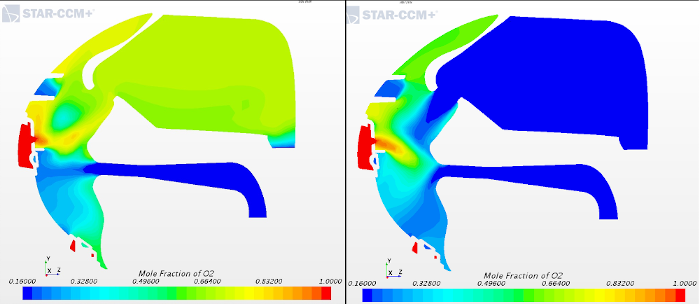
“Historically we were forced to use more simplified models, for example in the development of a respiratory mask, we would have used a simplified head model on our CFD simulations, with idealized breathing holes for the nose and the mouth,” explained Dr. Varga. “Although we were able to extract meaningful engineering data from those types of simulations, they don’t allow us to simulate all of our use cases realistically.”
For this reason, Varga set about improving the simulation process by gradually introducing more patient-specific data into CFD simulations:
“We are now using scans of real human heads that represent the morphologies of actual patient features. When it comes to respiratory simulations, we incorporate lung structure and volume using a variety of breathing profiles,” said Varga. “We are starting to build a library of patient morphologies, which already consists of representative patient geometries for all of the patient populations: adult, pediatric, and infant.”
In other words, the simulations account for “every stage of life.” Vyaire’s commitment to realistic simulation doesn’t stop there though; within those broad patient categories, Varga and his team are developing a complete library of patient morphologies and usage scenarios:
“For example, consider a patient who is sick or an elderly woman who has stiff lungs. We need to design devices that can be used for that patient as well as a more healthy patient, or perhaps even a highly tuned professional athlete with enormous lung capacity,” explained Dr. Varga. “Within each patient category, we are starting to build that out, from average to bariatric head models, so that we can simulate the entire spectrum of clinical usage.”
This seems very important in the context of the COVID-19 crisis, which is causing breathing difficulties in, and often hospitalizing, people of all shapes and sizes and from (almost) all demographic backgrounds:
“Simulation has brought to light a unique exploratory power for medical device engineers and researchers to design and build better solutions much more efficiently,” said Varga. “CFD already plays an important role in the front and the middle of our development cycle, and we expect increasingly to find a role in regulatory validation and verification. The power of simulation for medical device development has grown even greater with the capability to incorporate the patient into the simulation.”
Vyaire’s response to the crisis is impressive. The whole company has been working tirelessly to deliver ventilator equipment for patients in respiratory distress due to COVID-19 and to the healthcare workers treating them. Previously manufacturing 1700 ventilators per month, Vyaire is working around the clock to scale up their production exponentially. Every extra ventilator is potentially a life saved.
“Early in the development cycle, we extensively use CFD to achieve our feasibility goals through simulation rather than using time-consuming and expensive physical prototypes”, concluded Dr. Varga. “Having the capability to develop our products using Simcenter STAR-CCM+ allows us to significantly reduce development times and results in higher quality products and better patient outcomes.“
I’m always thrilled to be reminded that there are people alive that wouldn’t otherwise be without improvements that occurred as a direct consequence of innovations that are enabled through simulation.


Comments
Comments are closed.